|
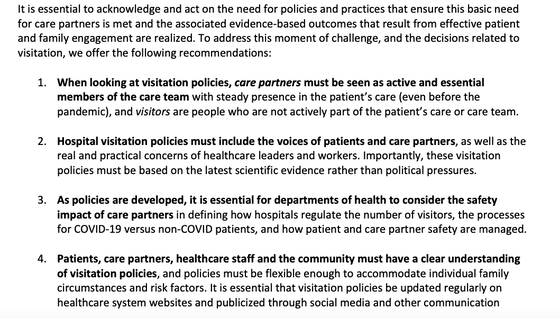
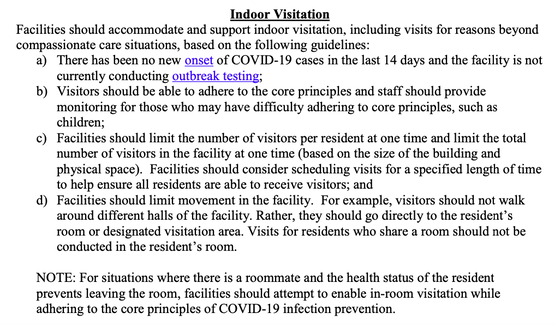
Thank you Betsy Phillips, Realtor, Baird & Warner, for having me on your "Let's Chat" series to talk about patient advocacy! Medicare's annual open enrollment period starts this month and that means there are A LOT of commercials urging people to switch plans. Here are some of my thoughts after seeing yet another one of those commercials...  I was recently on a podcast, hosted by Claudia Cometa of Peace Advocacy Group, with 3 other fabulous patient advocates. Listen to learn more about what patient advocates do. I talk specifically about how to talk to your aging parents about health and safety concerns and what has surprised me most about my work as a patient advocate.  Since the beginning of the pandemic, I’ve received many calls and heard many stories about how difficult the visitor restrictions continue to be for hospitalized patients, residents of senior living communities, and family members. As the pandemic continues, more and more organizations and individuals have been voicing concern about the isolation of seniors in assisted living and skilled nursing facilities, as well as the lack of advocacy for hospitalized patients. While exceptions for end-of-life or compassionate care visits have been available throughout (for patients without COVID), they often require families to make painful, difficult choices about who can say goodbye in person. Rules for all of the above scenarios have changed, loosened and also vary based on geographic area and facility. Be sure to check the most recent policy of the health care facility or community in question. Please use the information below to understand the issues as well as to advocate to visit your loved ones. Hospital/healthcare settings: The Beryl Institute recently released Patient and Family Recommendations for Addressing Visitation Policies during COVID-19. This policy statement emphasizes the importance of allowing a “care partner” to be in the hospital or any healthcare setting with patients. Anyone who has been in the hospital or had a loved one in the hospital knows how critical it is to have someone there with you: it’s usually difficult to understand and remember what the doctors are saying and ask meaningful questions when you are in a health crisis. Care partners also provide important information to health care providers that patients, due to physical illness, cognitive issues or just being overwhelmed, tired, or scared, may not remember to share on their own. While these recommendations include that “All patients must have the option to have a care partner present in the healthcare setting,” they also set out guidelines and responsibilities for care partners to keep healthcare personnel safe. The photo below shows some of the recommendations: Please see my previous post about having an “In Case Of Emergency Kit” prepared - this will make it easier for your care partner! Long term care settings: The Centers for Medicare & Medicaid Services (CMS), has issued guidelines to states regarding visitation of residents of long term care facilities. They note: While CMS guidance has focused on protecting nursing home residents from COVID-19, we recognize that physical separation from family and other loved ones has taken a physical and emotional toll on residents. Residents may feel socially isolated, leading to increased risk for depression, anxiety, and other expressions of distress. Residents living with cognitive impairment or other disabilities may find visitor restrictions and other ongoing changes related to COVID-19 confusing or upsetting. CMS understands that nursing home residents derive value from the physical, emotional, and spiritual support they receive through visitation from family and friends. The guidelines address indoor and outdoor visits as well as compassionate care visits and visitor testing. See the photo below for some of the guidelines for indoor visits. Check the guidelines from your state and the long term care facility you wish to visit for more specifics. Bottom Line: There should be ways to allow family members to advocate for and visit their loved ones, combat social isolation, and also prevent the spread of Covid-19. Hopefully, the recent progress in developing guidelines for visitors will help people get the care and companionship they need.
 I want to thank Jeffrey Wallk, The Value Enablement Group LLC, and Elizabeth Finlayson, The Non-Profit Coach, for featuring me on their Ask the Experts webcast. I shared information about my business as well as examples of how I’ve worked with clients, how I can help in different situations, and more. I often hear from clients that they feel dismissed by their doctors — that their doctor doesn’t care about them. Watch this quick video to learn how I helped a client turn this situation around.  How many of you have had a Telehealth appointment - either audio or video - since the COVID-19 pandemic started? I recently gave a presentation via Zoom to a group of about 25 older adults. I used the polling feature to ask if they’ve tried Telehealth and if they liked it. 80% reported that they had used it and thought it was great (the other 20% had not used it yet). Honestly, I was surprised at how many had used it AND liked it. This month’s blog provides some tips to make your Telehealth appointment successful. Telehealth may transform how healthcare is delivered in the future. It cannot replace every type of clinical visit, but in many cases, it can be just as good as being there in-person — just without the hassle of having to get to a doctor’s office. If the HIPAA rules and insurance reimbursement changes stay in effect even after the COVID-19 Public Health Emergency ends, we’ll all need to get familiar and comfortable with these type of provider appointments. It’s important to know that Telehealth was always subject to strict HIPAA privacy and confidentiality rules. Any platform used for Telehealth had to be HIPAA-compliant. These HIPAA rules have been relaxed since the Public Health Emergency was put in place; this means that providers and patients are using any form of communication that works, including FaceTime, Google Hangouts, whatever. Medicare has made some important changes to Telehealth. Currently, any provider who is eligible to bill for Medicare may provide and be reimbursed for services delivered as Telehealth. That includes doctors, nurses, mental health professionals, physical therapists, and more. They can bill patients for usual cost-sharing (co-pays, co-insurance) but they have the option to waive or reduce those fees. Also, the requirement that a patient had to see the provider in the past 3 years in order to have a Telehealth appointment is waived. Here are some tips to make Telehealth easier and more effective:
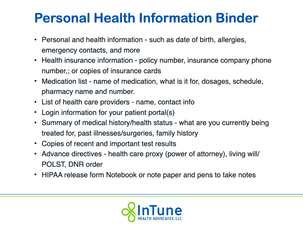
Today, April 16, is National Healthcare Decisions Day. It’s a day dedicated to helping people think about advance care planning - which is really about quality of life. If you’ve been reading my newsletters and keeping up with me on social media, you know that I often highlight the importance of getting your advance directives (health care proxy, living will, POLST) in order. The current situation with COVID-19 — heightened risk as well as a prohibition on having any visitors in hospitals, skilled nursing facilities, and senior communities — drives home this point even more. Spending time to get your important health information organized and sharing it with the appropriate people is critical to helping your health care proxy and family members advocate for you in an emergency. Keep reading below for more info. Stay well and stay home!
I’ve written before about creating a Personal Health Information Binder. Some people are calling it a “Grab and Go Kit” or “Emergency Health Kit.” Regardless of the name, the idea is the same: Organize your important health care-related information in a binder or folder. Keep a copy by your front door or somewhere where an EMT would see it and grab it to take with you to the hospital in case of an emergency; therefore, the front of it should say in big letters: TAKE IN CASE OF MEDICAL EMERGENCY. Also, make sure your health care proxy has a copy of all this information. If your health care proxy doesn’t live near you, make sure a trusted neighbor or friend knows that you have this folder and where it is in case someone needs to bring it to the hospital.
What should be in this folder/kit:
I also recommend keeping your cell phone fully charged and having an extra charger in your folder or binder. If you want to have a small bag prepared too, you could include extra hearing aids/batteries and glasses, if needed, as well as some toiletries. If you have not set up a patient portal, now is a great time to do that. In “normal times,” it’s an easy way to contact your doctors and keep track of your test results and upcoming appointments. Share the login information with your health care proxy and trusted family members in case they need more information to help advocate for your care. While you may think that the health care professionals taking care of you will have access to that information, it’s entirely possible that you might not be taken to your usual hospital. (2) Advance care planning is about control. In this time of so much uncertainty and fear, anything that gives us a sense of control can be comforting. It’s the perfect time to think about your wishes and who you want to be in charge of carrying them out for you, if necessary. Five Wishes is a national document accepted by almost all states. It includes a form to list your Health Care Power of Attorney but also includes an easy-to-use way for you to let people know what kind of care you would want. Other great resources include The Conversation Project and MyDirectives.com Feel free to contact me if you have questions about or need help with any of this -- gayle@InTuneHealthAdvocates.com or 847-920-8238. Surreal. Unprecedented. These are words we are hearing over and over to describe the current situation we are in. The vast majority of you reading this monthly newsletter live in a state that has already implemented a lockdown order. While I don’t think there’s much new I can add to what you have already read about how to prevent COVID-19 and what the symptoms are, I am sharing some important information below about how the health care system is being impacted and how that affects us personally.
Also, the need for advocacy in health care matters has not stopped during this time. InTune Health Advocates, LLC is still open for business… remotely. I am still calling health insurance companies and providers about surprise bills, denials, and billing errors; I am still helping families work through difficult decisions about discharge planning from hospitals and skilled nursing facilities; I am still helping clients research information about treatment options; and more. Important reminders and information:
|
AuthorWrite something about yourself. No need to be fancy, just an overview. Archives
February 2024
Categories |



 RSS Feed
RSS Feed



